Coronary artery spasm
The coronary arteries supply blood and oxygen to the heart. Coronary artery spasm is a brief, sudden narrowing of one of these arteries.
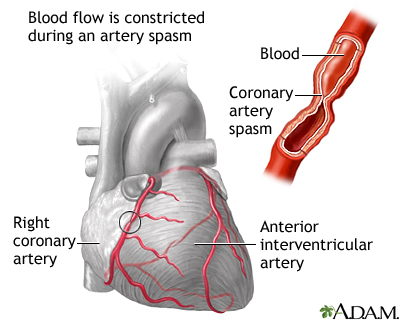
The spasm often occurs in coronary arteries that have not become hardened due to plaque buildup. However, it also can occur in arteries with plaque buildup.
These spasms are due to a squeezing of muscles in the artery wall. They most often occur in just one area of the artery. The coronary artery may appear normal during testing, but it does not function normally.
About 2% of people with angina (chest pain and pressure) have coronary artery spasm.

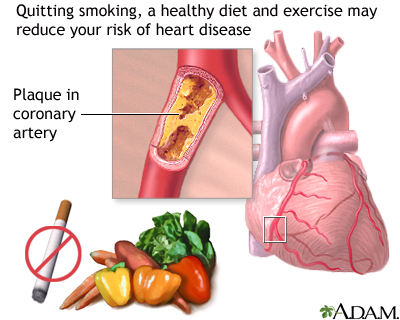
Coronary artery spasm occurs most commonly in people who smoke or who have high cholesterol or high blood pressure. It may occur without cause, or it may be triggered by:
- Alcohol withdrawal
- Emotional stress
- Exposure to cold
- Medicines that cause narrowing of the blood vessels (vasoconstriction)
- Stimulant drugs, such as amphetamines and cocaine
Cocaine use and cigarette smoking can cause severe spasms of the arteries. This causes the heart to work harder. In many people, coronary artery spasm may occur without any other heart risk factors (such as smoking, diabetes, high blood pressure, and high cholesterol).
Spasm may be "silent" (without symptoms) or it may result in chest pain or angina. If the spasm lasts long enough, it may even cause a heart attack.
The main symptom is a type of chest pain called angina. This pain is most often felt under the chest bone (sternum) or left side of the chest. The pain is described as:
- Constricting
- Crushing
- Pressure
- Squeezing
- Tightness
It is most often severe. The pain may spread to the neck, jaw, shoulder, or arm.
The pain of coronary artery spasm:
- Often occurs at rest
- May occur at the same time each day, usually between midnight and 8:00 a.m.
- Lasts from 5 to 30 minutes
The person may lose consciousness.
Unlike angina that is caused by hardening of the coronary arteries, chest pain and shortness of breath due to coronary artery spasm are often not present when you walk or exercise.
Tests to diagnose coronary artery spasm may include:
- Coronary angiography
- ECG
- Echocardiography
The goal of treatment is to control chest pain and prevent a heart attack. A medicine called nitroglycerin (NTG) can relieve an episode of pain.
Your health care provider may prescribe other medicines to prevent chest pain. You may need a type of medicine called a calcium channel blocker or a long-acting nitrate long-term.
Beta-blockers are another type of medicine that is used with other coronary artery problems. However, beta-blockers may make this problem worse. They should be used with care.
If you have this condition, you should avoid coronary artery spasm triggers. These include exposure to cold, cocaine use, cigarette smoking, and high-stress situations.
Coronary artery spasm is a long-term (chronic) condition. However, treatment most often helps control symptoms.
The disorder may be a sign that you have a high risk for heart attack or deadly irregular heart rhythms The outlook is most often good if you follow your treatment your provider's advice and avoid certain triggers.
Complications may include:
- Abnormal heart rhythms, which may cause cardiac arrest and sudden death
- Heart attack
Immediately call your local emergency number (such as 911) or go to the hospital emergency room if you have a history of angina and the crushing or squeezing chest pain is not relieved by nitroglycerin. The pain may be due to a heart attack. Rest and nitroglycerin do not completely relieve the pain of a heart attack.
A heart attack is a medical emergency. If you have symptoms of a heart attack, seek medical help right away.
Take steps to reduce your risk of heart disease. This includes not smoking, eating a low-fat diet, and increasing exercise.
Variant angina; Angina - variant; Prinzmetal's angina; Vasospastic angina; Chest pain - Prinzmetal's
Anderson JL, Adams CD, Antman EM, Bridges CR, et al. 2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction. Circulation. 2013;127(23):663-828. PMID: 23630129 www.ncbi.nlm.nih.gov/pubmed/23630129.
Boden WE. Angina pectoris and stable ischemic heart disease. In: Goldman L, Schafer AI, eds.Goldman's Cecil Medicine. 25th ed. Philadelphia, PA: Elsevier Saunders; 2016:chap 71.
Giugliano RP, Cannon CP, Braunwald E. Non-ST elevation acute coronary syndromes In: Mann DL, Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 10th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 53.
Updated by: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Isla Ogilvie, PhD, and the A.D.A.M. Editorial team.




